Infertility Treatment
THE FEMALE REPRODUCTIVE SYSTEM:
The Female Reproductive system consists of the following parts:
• Ovaries
• Fallopian Tubes
• Uterus
• Cervix
• Vagina
OVARIES:
Each ovary is about the size of an unshelled almond. It releases eggs, called ovum every month. It also produces female sex hormones, control the menstrual cycle as well and produces and maintains the secondary sexual characteristic such as breasts. The ovaries contain 2 million immature eggs at birth itself. One immature egg matures every month after a female child reaches 12 years. It takes around a thousand tail strokes to drive a sperm forward by a centimeter.
Sperms are helped on their way by contraction of the uterus, which forces them upwards into the body. The contractions are stimulated by prostaglandins (hormones) contained in the semen. At most times of the monthly cycle, sperms may not reach the uterus at all, as it is kept out by a plug of impenetrable mucus around the cervix. Only at the time of ovulation, the cervical mucus become loose and allows the sperm to pass through. Once in the vicinity of the egg, the sperm is chemically attracted to it. When they reach their destination,they must first penetrate the corona radiata. The sperm release certain enzyme that dissolves the corona radiata. This allows the head of the sperm to burrow downwards towards the egg cell. This journey takes about 30 minutes. Once the sperm is inside, it releases a chemical signal that activates the egg. The sperm head is drawn towards the nucleus of the egg, and their genetic material fuses.
FALLOPIAN TUBES:
The egg and the sperm meet in the fallopian tubes. For normal conception, the tubes should not be blocked
UTERUS:
The inner lining of the uterus should be conducive for implantation of the embryo. If it is thin, the embryos will not implant or if there is any hindrance like septa, polyp, fibroid or adhesion, the embryo will not implant. So before starting treatment, hysteroscopy is mandatory to check the uterine cavity.
CERVIX:
The cervix is the entrance to the uterus. It is a “gate way” for sperm to enter the uterus.
VAGINA:
It is a muscular tube about 3” – 4” in length. It is an exit route for the discarded endometrium during menstrual periods, and for the baby during birth.
MENSTRUATION:
Menstruation is the natural loss of blood and cellular debris from the uterus. It usually occurs at monthly intervals throughout the reproductive life of a woman. It is commonly referred to as period. Each month there are 2 events taking place; ovarian and menstrual events. Both these events are responsible respectively, for the release of an egg from an ovary, and preparation of the uterus to receive the egg. Both the cycles last on an average, for 28 days.
HORMONES INVOLVED IN OVARIAN CYCLE:
The ovarian cycle is controlled by two pituitary gland hormones: Luteinizing hormones (LH) and follicle stimulating hormones (FSH) FSH stimulates some follicles (Sacs) containing immature egg to grow and mature. Eventually one follicle and its egg become larger than the others. In the mid cycle, LH levels rise and cause ovulation. The follicle bursts, releasing its egg into the uterine tube. If the egg is not fertilized, a new ovarian cycle starts 14 days after ovulation.
HORMONES INVOLVED IN MENSTRUAL CYCLE:
The menstrual cycle causes a thickening of the endometrium, the inner lining of the uterus, in readiness to receive the fertilized egg. FSH stimulates the ovary to release estrogen, which stimulates endometrial thickening.
FOLLOWING OVULATION, THE OVARY ALSO SECRETS PROGESTERONE:
Both estrogen and progesterone together stimulate further thickening of the endometrium. If fertilization does not happen, progesterone and estrogen level drops, the endometrium fragments sheds and a woman get her period
LAPROSCOPY IN INFERTILITY:
Laparoscopy is a type of surgical procedure that allows a doctor to observe a woman’s uterus, ovaries and a fallopian tube. It is often used to detect ovarian cysts, fibroids, scar tissue, and diagnose pelvic or abdominal pain, endometriosis, ectopic pregnancy or blocked fallopian tubes. Laparoscopic surgeries are usually done as a day care procedure under general anaesthesia. The viewing tube (called the laparoscope) is equipped with a small camera on the eyepiece and is inserted through a small incision in the naval. The doctor can then examine the abdominal and pelvic organs on a video monitor connected to the tube. Other small incisions can be made to insert instruments to perform a variety of procedures. Laparoscopy is less invasive than regular open abdominal surgery (laparotomy).
IUI:
Intrauterine Insemination (IUI) is a common procedure performed in cases of cervical hostility, erectile dysfunction and unexplained infertility. In this procedure, sperms are placed inside the uterine cavity after preparation of the sample. It is mandatory, to have the tubes open for this particular procedure. If the tubes are blocked patient has to resort to ‘test tube’ baby only. This procedure does not require hospitalization.
IUI IS USEFUL WHEN:
-The woman has a cervical mucus problem. For example, it may be scanty or hostile to the sperm. With an intrauterine insemination, the sperm bypass the cervix and enter the uterine cavity directly.
-The man has antibodies to his own sperm. The “good’ sperm which have not been affected by the antibodies are separated in the laboratory and used for IUI.
-If the man cannot ejaculate into his partner’s vagina. This is usually because of psychological problems such as impotence (inability to get and maintain an erection) and vaginismus (an involuntary spasm of the vaginal muscles so that vaginal penetration is not possible); or anatomic problems of the penis, such as uncorrected hypospadias or if he is paraplegic.
-The man suffers from retrograde ejaculation in which the semen goes backward into the bladder instead of coming out of the penis.
-For unexplained infertility, since the technique of IUI increases the chances of the egg and sperm meeting.
-IUI is a reasonable first choice (especially for younger couples) since it is so much cheaper and less intrusive.
-For male factor infertility, though this is a controversial area, especially for the common problem of oligospermia (a low sperm count). What is the rationale behind using IUI for treating this problem? Remember that infertility is a problem of the couple’s, not just male’s oligospermia. Whether a given couple will conceive or not depends on the sum of their fertility potentials. Therefore, the fertility potential of the wife is improved by superovulating her, so that instead of producing 1 egg per cycle, she produces 2-4 eggs per cycle. In addition, the husband’s sperms are processed in the laboratory and the best sperms are used for IUI. This increases the chances of the best sperm being able to reach and fertilize the egg.
HOW WELL IT WORKS:
Insemination procedures can improve your chances of becoming pregnant, especially when combined with superovulation treatment. Treatment success is strongly influenced by a women’s age (an aging egg supply decreases pregnancy rate, and miscarriage risk increases with age).
TREATING MALE SPERM PROBLEMS:
For mild male infertility, one cycle of IUI has produced double the pregnancy rate (6.5%) of that of well-timed intercourse (3%). Superovulation is reported to only slightly increase the chance of conception when using IUI for mild male infertility
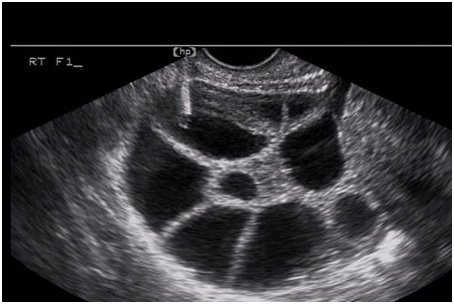
FOLLICULAR STUDIES:
Follicular monitoring or follicular study is a vital component of in-vitro fertilization (IVF) assessment and timing. It basically employs a simple technique for assessingovarian follicles at regular intervals and documenting the pathway to ovulation.
Physiology
Journey to ovulation begins during late luteal phase of prior menstrual cycle, when certain 2-5 mm sized healthy follicles form a population, from which dominant follicles is to be selected for next cycle This process is called 'recruitment'. Usual number of such follicles may be 3-11, which goes on decreasing with advancing age1.
During Day 1-5 of the menstrual cycle, a second process of 'follicular selection' begins, when among all recruited follicles, certain growing follicles of size 5-10 mm are selected, while rest of the follicles regress or become atretic.
During Day 5-7 of the menstrual cycle, a process of 'dominance' begins, when a certain follicle of 10 mm size takes the control and becomes dominant. This also suppresses the growth of the rest of the selected follicles, and in a way, is destined to ovulate. This follicle starts growing at rate of 2-3 mm a day and reaches 17-27 mm size just prior to ovulation 2. One important learning point in this regard is, "largest follicle on day 3 of the cycle, may or may not be a dominant follicle in the end. Process of dominance begins late, when suddenly a certain underdog follicle starts growing faster and suppresses others to become dominant".
Almost nearing ovulation, rapid follicle growth takes place, and follicle starts protruding from the ovarian cortex, attains a crenated border, and it literally explodes to release the ovum, along with some antral fluid.
Ultrasound Monitoring: General
Transvaginal ultrasound is preferred and usually mandatory modality for monitoring follicles. Ultrasound monitoring may begin on day 3 of the cycle, to assess a baseline size, as well as exclude if any cyst remains from previous hyperstimulation or otherwise. Its important to count the number of existing follicles, document two/three dimensions of each follicles, and also comment on shape (round/oval/rectangular/triangular), echogenicity (echogenic/hypoechoic/anechoic) and antral edges (smooth/intermediate/rough) if possible.
As the study progresses on day 7, we should start guessing the ovulatory dominant follicle i.e. dominant follicle which is destined to ovulate. Basically, there are three varieties of eligible follicles:
1. atretic dominant follicle: This follicle is usually largest follicle on day 3, but it is not destined to ovulate. It has an irregular shape, rough edges, and may be little echogenic.
2. ovulatory dominant follicle: This follicle is typically round, with smooth borders, and usually hypoechoic.
3. anovulatory-luteinizing dominant follicle: This dominant follicle grows at a good pace but fails to ovulate, and later becomes a cyst or luteinizes. These are also round and smooth, however anechoic. This subtle recognition of echogenicity difference between hypoechoic and anechoic follicle can help determine whether a follicle is growing to ovulate.
Once the follicle reaches 16 mm size, a daily monitoring of follicle is recommended.
Next step is documentation of ovulation. Ovulation is sonographically determined by following sonographic signs:
1. follicle suddenly disappears or regresses in size
2. irregular margins
3. intra-follicular echoes. Follicle suddenly becomes more echogenic
4. free fluid in the pouch of Douglas
5. increased perifollicular blood flow velocities, on doppler
Hospital Location
1st Floor, Riddhi Residency, Above SBI Bank, Near TGB Restaurant, LP Savani School Main Road, Adajan Surat.+91-0261-2746100/200
info@shubhamhospital.co.in
Copyright © Shubham Hospital - 2016
By - e2Sigma
